Individual results may vary. Rx Only. View important safety information at inspiresleep.com/safety.
What is obstructive sleep apnea?
Learn what obstructive sleep apnea (OSA) is, its causes, symptoms, risks and treatments, including FDA-approved therapies, to improve sleep and overall health.
Topics
People often think excessive snoring, waking up repeatedly while trying to sleep and consistently feeling too tired to do daily tasks are normal. However, these may all be signs of obstructive sleep apnea (OSA), a sleep disorder with serious health risks. OSA affects an estimated 30 million people in the United States and 1 billion globally.1, 2 And most people – up to 90% – who have OSA don’t know it.3
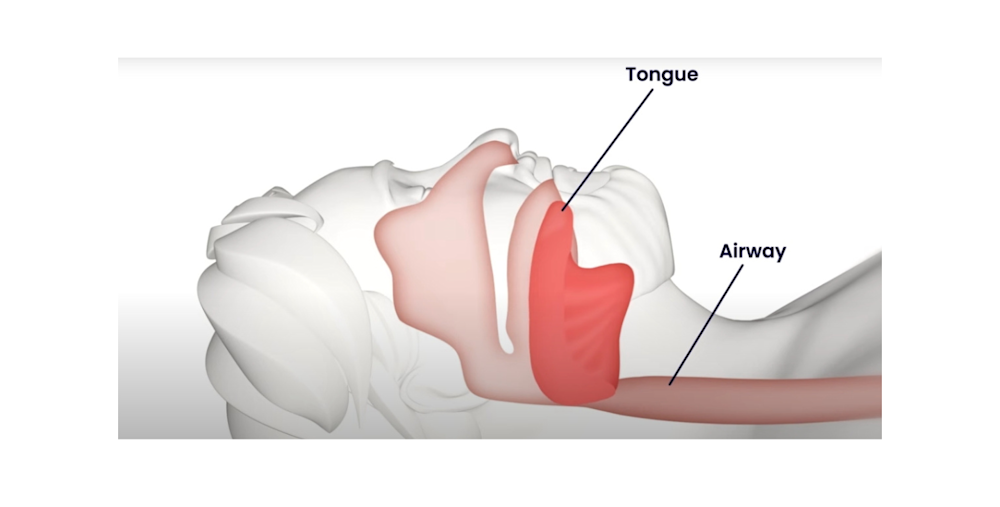
When you have OSA, your tongue relaxes back into your airway during sleep and blocks airflow, making it difficult – or even impossible – to breathe regularly. These “sleep apnea events” can happen repeatedly for short periods throughout the night. Each time one does, your brain alerts you to wake up and take a breath. If this happens to you five or more times per hour, it prevents you from getting the deep, restorative sleep your body and mind need.
Overall health and well-being require quality sleep
For adults, it’s generally recommended to get 7 to 9 hours of quality sleep per night. Without enough sleep, it gets harder and harder to get through the day or maintain your long-term health. It can be difficult to concentrate, stay alert, be physically active or mentally productive, too. Many people feel like a shell of themselves – crabby, short tempered and/or drained. These changes in how you feel, your behavior and attitude can also affect your relationships, job performance and your overall quality of life.
On a physical level, the ongoing breathing interruptions make it harder for your body to get enough oxygen. This puts stress on your vital organs, like your heart, lungs and brain, and raises the risk of serious medical conditions like hypertension (high blood pressure), stroke, heart failure, diabetes and depression. It can also make existing health conditions worse and weaken your immune system.
That’s a lot to take in, let alone manage on your own. Rest assured, OSA is treatable – and many people who follow their care plan sleep better, feel like themselves again and live full lives.
It’s important to get a proper diagnosis and a treatment plan. Here’s a quick overview to get you started on the journey.
What is OSA?
You might’ve heard of “sleep apnea” as a general term. There are three main types of sleep apnea: OSA, which is the most common, central sleep apnea (CSA) and complex sleep apnea (CompSA), which is a combination of OSA and CSA. In each case, your breathing stops and starts for short periods while you’re asleep, making it harder for your body to get enough oxygen and stressing your vital organs.
The key difference among the three types is what is causing your disrupted breathing. With OSA, as mentioned above, your airway gets partially or completely blocked because your tongue (or other soft tissue in your throat) collapses and obstructs your airway.
With CSA, to put it simply, your brain sometimes fails to signal you to breathe while you’re sleeping. How often depends on the severity of your condition.
The tricky part is OSA and CSA symptoms overlap with each other and with other sleep disorders, like insomnia and narcolepsy. This can make it harder to identify which condition you have without a thorough examination and proper diagnosis. Both OSA and CSA may lead you to:
Wake up gasping for air
Have trouble falling and/or staying asleep
Feel exhausted during the day
Wake up with a dry mouth, sore throat or headache
Sleep restlessly, including tossing and turning or getting up to use the toilet
Have difficulties with focus and/or your memory
Have a decreased sex drive
Have mood swings and other changes in behavior
These are some of the common symptoms, but each person may have a different experience.
What causes OSA?
Another difficult aspect of diagnosing OSA is it can affect both children and adults, as well as people from any background. So, even if you don’t fit the typical profile, it doesn’t mean you don’t or can’t have it. However, OSA is most commonly associated with:
Males
Older adults
Being overweight or having obesity
Cardiovascular, metabolic, neurological or respiratory conditions, including congestive heart failure, high blood pressure, type 2 diabetes, hormone disorders, prior stroke or chronic lung diseases like asthma
A family history of OSA
Enlarged tonsils or adenoids, a narrow or blocked upper airway, thick neck, or weakened neck and/or airway muscles
Down syndrome
In addition, substances – such as cigarettes, alcohol, sleeping pills and opioid pain relievers – can relax the muscles in your throat, making it harder to breathe and increasing your risk of developing OSA. They can also make existing OSA symptoms more severe.
How is OSA diagnosed?
To diagnose OSA and other sleep disorders, a provider typically gathers information about your symptoms, medical history and lifestyle. They may also talk to someone in your household who can describe symptoms you might not notice, like if you stop breathing during sleep, snore loudly or act differently. A physical exam is usually done to identify potential OSA risk factors or complications, like high-blood pressure, nasal congestion or excess weight.
If these preliminary evaluations suggest the potential of OSA, your provider will likely recommend a sleep study (also called a “polysomnography”) in a lab or a home sleep test. A sleep specialist will monitor your brain activity, eye movement, heart rate, breathing, airflow and blood oxygen levels to check for OSA while you sleep. If they identify between 5 and 15 sleep apnea events per hour, it’s considered mild OSA. Between 15 and 30 times per hour is moderate and more than 30 times per hour is severe.
Your provider will discuss treatment options with you based on your results, age, overall health, insurance coverage and lifestyle factors.
What can you do to help reduce your symptoms?
The first line of defense is often to address behaviors (also referred to as lifestyle choices) that may help reduce your OSA symptoms. This may include encouraging you to stop smoking, drinking alcohol or taking sedatives, being more active, losing excess weight, and improving your sleep schedule and environment.
If you’re already on a care plan for an existing health condition, they will review it (and, if needed, collaborate with the relevant care team) to be sure you’re following it and to consider any modifications that may help you. They may also recommend “myofunctional therapy,” which involves exercises to strengthen the tongue, mouth and throat muscles to help improve breathing.
These types of changes may help reduce OSA symptoms, especially in mild cases. Dental appliances like mouthpieces can also be used to reposition the jaw and tongue to help improve breathing and reduce sleep apnea events in mild cases.
What are the medical treatments for OSA and when are they used?
For moderate and severe OSA conditions, many people usually need additional medical intervention. Usually, the first prescribed is a continuous positive air pressure (CPAP) machine. It’s a system that delivers air directly into your airway. It does this through a hose attached to a mask that’s attached over your nose and mouth. It’s meant to keep your airway open during sleep, so you can breathe more easily. About half of patients4,5 prescribed CPAP therapy struggle with it or stop using it. And, left untreated, OSA leaves them at risk for serious health problems, as outlined above.
For those who are unable to tolerate or find benefit from CPAP, Inspire® therapy is another option. It’s the leading – and longest in use – FDA-approved nerve stimulation therapy for treating OSA. It’s been proven to reduce the number of sleep apnea events by up to 79%6 and more than 100,000 people have trusted it to treat their OSA.7
Different from other OSA treatments, Inspire therapy is a mask-free8 solution that works comfortably9 inside your body to treat the root cause of OSA. The small Inspire® implant, placed under your skin near your collarbone during a short outpatient procedure, delivers gentle pulses to your airway muscles while you sleep. These pulses help keep your airway open, so you can breathe regularly and sleep soundly. You use a small remote control to turn the therapy on and off.
Finally, if you have structural issues with your nose, mouth, throat or jaw that get in the way of airflow, your provider may recommend a surgical procedure. The specific type of surgery would depend on your unique needs, but it often involves repairing airway-related structures or removing tissue that blocks airflow. These types of surgeries are usually considered a last resort when other treatments haven’t been effective, as they tend to carry more risk and require a longer recovery time.
Talk to a healthcare provider
If you’re concerned you or someone you care about might have obstructive sleep apnea (OSA), rest assured, it’s treatable. It’s important to seek medical advice, such as from a primary care provider. Left untreated, OSA can lead to serious health risks or worsen existing ones. Many people find a treatment that fits their lifestyle, helping them manage their condition and enjoy fulfilling lives.
Sources
Cleveland Clinic, Sleep Apnea: What It Is, Causes, Symptoms & Treatment. January 15, 2025.
American Medical Association, What doctors wish patients knew about sleep apnea. April 1, 2022.
Johns Hopkins Medicine, Obstructive Sleep Apnea. Accessed April 10, 2025.
Rotenberg et al. Trends in CPAP adherence over twenty years of data collection: a flattened curve. Journal of Otolaryngology Head and Neck Surgery 2016; 45:43
Weaver, TE, Sawyer, AM. "Adherence to Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea: Implications for Future Inventions." Indian Journal of Medical Research, 2010; 131: 245-258.
Woodson BT, Strohl KP, Soose RJ, et al. Upper Airway Stimulation for Obstructive Sleep Apnea: 5-Year Outcomes. Otolaryngology Head Neck Surgery 2018; 159(1):194-202).
Data on file.
ADHERE Registry: Data on File.
Suurna MV, Steffen A, Boon M, et al. Impact of Body Mass Index and Discomfort on Upper Airway Stimulation: ADHERE Registry 2020 Update. Laryngoscope 2021; 131(11): 2616-2624
HealthHub, Obstructive Sleep Apnoea. July 29, 2021.
HealthHub, The Importance of Sleep. November 15, 2022.
Mayo Clinic, Obstructive sleep apnea - Symptoms and causes. July 14, 2023.
Mayo Clinic, Sleep apnea - Symptoms and causes. April 6, 2023.
Sleep Foundation, Obstructive Sleep Apnea: Symptoms, Causes, and Treatments. April 16, 2024.
Sleep Health Foundation, Surgery for Obstructive Sleep Apnoea (OSA). Accessed April 10, 2025.
The University of Kansas Health System, Sleep Apnea Surgery. Accessed April 10, 2025.