Individual results may vary. Rx Only. View important safety information at inspiresleep.com/safety.
What are the most common causes and risk factors of sleep apnea?
Learn the signs and symptoms, risk factors and how lifestyle choices and medical conditions may contribute.
Topics
If you regularly have trouble sleeping, there could be many reasons. Stress is a common one. So are keeping an unpredictable schedule, eating and drinking too close to bedtime, and sharing a bed with someone who snores. Then again, you may also be waking up periodically through the night just to breathe – without even realizing it.
Any of these can leave you exhausted. But the last one is a sign of sleep apnea, a serious medical condition that affects an estimated 1 billion people globally.1,2 While some causes of poor sleep can be improved with small changes in your routine, sleep apnea needs to be diagnosed and treated by a doctor.
Beyond ruining a good night’s sleep, untreated sleep apnea increases your risk for serious health conditions. These include cardiovascular issues (such as high blood pressure, heart attack, stroke and heart disease), obesity, type 2 diabetes and depression.
If you already have one of these conditions, sleep apnea can make it harder to manage, too. Because sleep apnea leaves you feeling tired all the time, it can also strain your relationships and work performance, and increase your risk of injuries and accidents.
In addition, many medical conditions can increase your risk of developing sleep apnea. These include congestive heart failure, high blood pressure, type 2 diabetes, hormone disorders, prior stroke, chronic lung disease like asthma, obesity and Down syndrome.
Signs you may have sleep apnea
How do you know if you have sleep apnea? That’s a good question. Common signs and symptoms of sleep apnea include:
Stopping breathing, snoring or gasping for air during sleep.
Frequently waking up with a dry mouth, sore throat or headache.
Feeling exhausted, falling asleep or napping during the day.
Finding it hard to focus or remember things.
Frequently getting common colds.
Decreased sex drive.
Behavior and attitude changes, like mood swings, irritability or quick temper.
It’s important to note, people experience sleep apnea in different ways. For example, not everyone with sleep apnea snores – and not everyone who snores has sleep apnea. If you’re regularly not sleeping well, it could be due to another type of sleep disorder, a mental health concern or something else entirely.
That’s why it’s important to talk to a medical provider for a proper diagnosis.
Types of sleep apnea, causes and risks
There are three types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA) and mixed or combined sleep apnea (CompSA). Typically, a sleep study is done to figure out what kind of sleep apnea you have and how serious it is.
OSA is the most common type of sleep apnea. It occurs when the tongue relaxes back into your airway during sleep, causing your airway to narrow or close and blocking your breath. When this happens, your body triggers you to wake up and take a breath or gasp for air. These interruptions, called “sleep apnea events,” can happen repeatedly throughout the night, preventing you from getting the quality sleep you need.
OSA can affect anyone of any background or age, including children. But it’s more common in males, older adults, people with a family history of it and people who are significantly overweight or have obesity. The shape and structure of your nose, throat or airway can also increase the risk of developing OSA. This includes things like big tonsils or adenoids, a smaller airway, a thick neck, or weak muscle tone in the throat or neck. Having OSA may raise your risk for other health concerns, or OSA can develop because of existing medical conditions.
The good news is, OSA is treatable. The treatment recommendation will be based on the results of your sleep study, the number of OSA events you experience and your symptoms. Providers typically break OSA conditions into three groups: mild, moderate and severe.
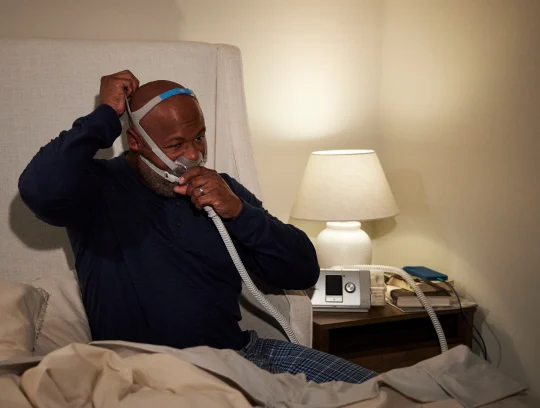
While changes in your lifestyle and behavior – such as quitting smoking, losing excess weight if you are overweight and maintaining a regular sleep schedule – can often help reduce symptoms, many people need medical treatment, too.
These may include wearing dental appliances, using continuous positive airway pressure (CPAP) systems, undergoing surgery to improve airflow, or implanting the Inspire® therapy device to help you breathe regularly and improve sleep. Note: Inspire therapy is the leading FDA-approved hypoglossal nerve stimulation therapy for OSA. It’s a mask-free3 solution for people with OSA who have tried and struggled with CPAP.
CSA is far less common. It happens if your brain doesn’t properly control your breathing during sleep. As you take fewer breaths or stop breathing for short periods, the oxygen and carbon dioxide levels in your bloodstream get out of balance. When they dip too low, your brain eventually signals you to take a breath, which results in you briefly waking up.
In many cases, the reason someone has CSA is unclear, but it could be something you’re born with or that develops due to other factors, such as a medical condition. CSA is most common among males aged 60 or older, particularly those with a heart, brain, spine or nerve disorder. Other risks include living at high altitudes and opioid use.
Like OSA, CSA is treatable and is typically diagnosed by reviewing your current health and conducting a sleep study to identify sleep apnea events.
Providers typically address any underlying or co-occurring conditions, such as heart failure, encourage lifestyle adjustments (like avoiding alcohol and sedatives, and sleeping on your side) and prescribe a CSA-specific treatment. This often includes a pressurized air system to help regulate breathing, such as a bilevel positive airway pressure (BiPAP) or adaptive servo-ventilation (ASV) device.
The third type of sleep apnea is a combination of OSA and CSA, called complex or mixed sleep apnea (CompSA). Its symptoms, causes and risk factors are similar to the ones above, depending on the individual.
With any sleep apnea disorder, it’s important to follow the guidance of your healthcare provider and adhere to your care plan.
Getting the care you need
Getting enough quality sleep is important to your overall health and wellness. It also plays a big role in helping you feel good and be more alert during the day. The following strategies can help improve sleep and, if you’re diagnosed with sleep apnea, may help manage your symptoms along your provider’s recommended treatment plan:
Practice self-care, including eating nutritious foods, being physically active and managing stress.
Follow a sleep routine with consistent bedtimes and a comfortable environment.
Maintain a healthy weight.
Avoid smoking, alcohol and sedatives.
Keep up with recommended preventive care like checkups and screenings.
Follow any current treatment plans you’re on for sleep apnea and other conditions.
If you are regularly struggling to get a good night’s sleep, or think you may have sleep apnea, it’s important to reach out to a healthcare provider or mental health professional. They can help identify what may be causing your sleep difficulties and connect you to the right support and treatment.
Sources
Cleveland Clinic, Sleep Apnea: What It Is, Causes, Symptoms & Treatment. January 15, 2025
American Medical Association, What doctors wish patients knew about sleep apnea. April 1, 2022.
ADHERE Registry: Data on File
Cleveland Clinic, Central Sleep Apnea: What It Is, Causes, Symptoms & Treatment. January 27, 2024.
Johns Hopkins Medicine, The Dangers of Uncontrolled Sleep Apnea. April 7, 2025.
Johns Hopkins Medicine, Sleep Apnea. April 7, 2025.
Mayo Clinic, Insomnia - Symptoms and causes. January 16, 2024.
Mayo Clinic, Sleep apnea - Symptoms and causes. April 6, 2023.
Medline Plus Medical Encyclopedia, Central sleep apnea. August 29, 2023.
Nature, Obstructive sleep apnea -related hypertension: a review of the literature and clinical management strategy. August 29, 2024.
NIH, National Heart, Lung and Blood Institute, Sleep Apnea - What Is Sleep Apnea? January 9, 2025.
Sleep Health Foundation, Common Causes of Inadequate Sleep. January 12, 2024.