Individual results may vary. Rx Only. View important safety information at inspiresleep.com/safety.
Sleep apnea and work: Risks, safety, and treatment
Discover how obstructive sleep apnea impacts job performance and safety. Learn symptoms, risks and treatment options to protect your health and livelihood.
Topics
Is sleep apnea affecting your job?
Struggling to keep your eyes open during a conference call. Losing focus while operating equipment or falling asleep at the wheel… Most jobs require alertness, clear thinking and coordination. A chronic lack of quality sleep can undermine these abilities – and put your health and livelihood at risk. The danger is especially high in safety-sensitive professions like driving, aviation and surgery.
Why alertness matters at work
Research shows that:
Employees with obstructive sleep apnea (OSA) or excessive daytime sleepiness are twice as likely to have workplace accidents.1
Commercial drivers with OSA disorder are seven times more likely to be involved in an accident than those without OSA.2
Fatigue likely contributed to 21 to 23 percent of major aviation accidents over a 20-year period.3
Sleep-deprived surgeons take longer to complete procedures.4
Employees experiencing a long-term lack of sleep can lose 40 to 50 percent of productivity compared to well-rested colleagues.5,6
Understanding obstructive sleep apnea
Sleep disorders are a leading cause of ongoing sleep loss – and obstructive sleep apnea is among the most common.
In fact, it’s estimated up to 30% of adults have obstructive sleep apnea – but the vast majority don’t know they do. 7,8,9 This happens for many reasons, including underestimating consistent poor sleep, and the fact that women and people of color are often underdiagnosed or misdiagnosed.
What is OSA?
When you have OSA, your airway becomes blocked during sleep because your tongue and other throat muscles and tissues relax and fall backward. This causes you to stop breathing, so your brain alerts you to wake up and take a breath. You may not remember waking up, but this cycle can happen repeatedly throughout the night – even hundreds of times for some people with severe OSA.
Health and safety consequences
Over time, these frequent awakenings can lead to chronic sleep deprivation, increasing the risk of accidents, injuries and serious health conditions, including high blood pressure, cardiovascular disease, obesity and depression. They also make it harder for your body to get enough oxygen, putting stress on your heart, lungs and brain.
Who’s at risk?
Obstructive sleep apnea can affect anyone of any background, but is most often diagnosed in older white men who are overweight and snore loudly. It’s also more prevalent among some groups – like commercial truck drivers10 – than in the general population.
It’s also important to note: Women and people of color are often underdiagnosed or misdiagnosed when it comes to sleep apnea.11,12 They’re also less likely to be screened for sleep apnea or referred to a specialist.
Symptoms to watch for
Every person’s specific experience may differ. Some people with OSA snore loudly, wake up with a sore throat, experience headaches, feel cranky and short tempered. Many feel drained during the day and have a hard time staying awake, focusing or getting things done. Because of this, some end up skipping work, school or daily commitments (absenteeism), while others show up but underperform (presenteeism).
Long-term, living with untreated OSA often changes how you feel, your behavior and attitude, which can affect your relationships, job performance and attendance, and overall health and quality of life.
Pursuing better sleep
These are all reasons why it’s crucial to pay attention to how you sleep – and feel – day to day, and consult with a medical professional if you notice a pattern of severe fatigue or disrupted sleep. With the right diagnosis and treatment, many people effectively manage their sleep apnea – and improve their overall health and well-being.
Common treatment options for OSA
There are a variety of effective treatment options for obstructive sleep apnea and other sleep disorders. Your doctor can make a recommendation based on your symptoms, medical history, insurance coverage and lifestyle needs.
Lifestyle changes
Many treatment plans begin with lifestyle changes, such as adjusting your sleeping position, losing excess weight, increasing physical activity, and avoiding smoking, alcohol and substance use. While these changes won’t necessarily cure sleep apnea, they can help reduce the severity of sleep apnea, especially in mild to moderate conditions.
However, many people need additional treatment.
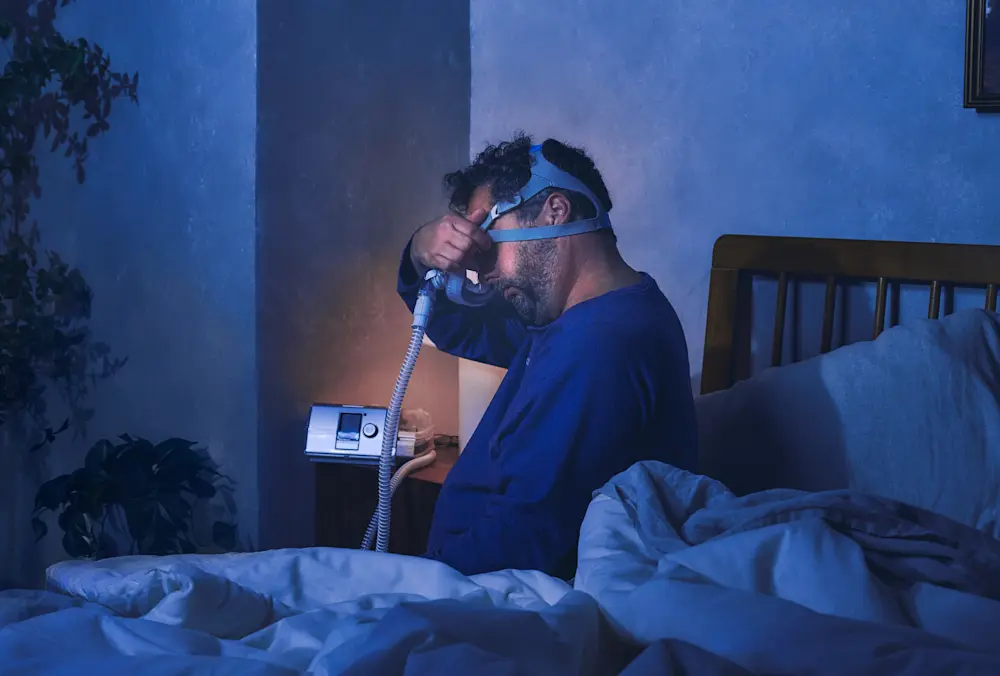
CPAP: Benefits and challenges
A continuous positive air pressure (CPAP) machine is commonly prescribed for people with moderate to severe sleep apnea. It’s a device that delivers air through a hose and mask to help keep the airway open during sleep.
It’s important to note: About half of patients13,14 prescribed CPAP therapy struggle with or stop using it. They find the mask uncomfortable or restricting, and struggle with the required maintenance. Some people also feel self-conscious using the system, and some bed partners find the machine disturbing.
Inspire® therapy: A mask-free15 option
When CPAP isn’t working, many people with sleep apnea become interested in Inspire therapy. Inspire therapy is an implantable, mask-free solution that works inside your body to treat the root cause of obstructive sleep apnea, so you can breathe regularly and sleep soundly.
It’s one of the most chosen next-line options – and 91% of Inspire patients say Inspire therapy is better than CPAP.16
Other treatment options
A variety of additional treatment options are available for sleep apnea to help improve breathing. These include mouthpieces that reposition the jaw and tongue, medications that support weight loss when excess weight contributes to symptoms and surgeries to adjust the structure of the nose, mouth, throat or jaw. Their suitability and effectiveness vary depending on your sleep apnea symptoms, medical history and other factors. New therapies are also emerging and becoming available. Talk to your healthcare provider to understand which options may be best for you, considering the pros and cons, proven effectiveness, success rates and insurance coverage.
Both CPAP and Inspire therapy are proven to be safe and effective treatment options for obstructive sleep apnea. And they both offer strong insurance coverage options by commercial plans, Medicare and Veterans Affairs (VA).
Compliance matters for safety-sensitive jobs
It’s important to note: Some occupations require employees with OSA to provide proof you’re following your prescribed treatment plan to manage the condition. This includes commercial drivers, pilots, train operators and some medical professionals. For both Inspire therapy and CPAP, your doctor can provide your usage record to submit to your employer.
Pursuing better sleep
Untreated OSA can significantly impact your health, safety and quality of life. If you experience symptoms like loud snoring, daytime fatigue or difficulty concentrating, consult with a healthcare professional. With proper diagnosis and treatment, many individuals manage OSA effectively and improve their overall well-being.
Sources
AJMC, Workers With Excessive Daytime Sleepiness, OSA at Higher Risk of Occupational Accidents. April 9, 2020.
FMSCSA, Evaluation of Research on CMV Drivers with Moderate to Severe Obstructive Sleep Apnea. May 30, 2024.
American Academy of Sleep Medicine, Taking steps toward safer skies. February 25, 2025.
PubMed, Impact of sleep deficiency on surgical performance: a prospective assessment. April 1, 2023.
Sleep Foundation, Sleep & Job Performance: Can Sleep Deprivation Hurt Your Work? July 22, 2025.
Journal of Health Economics and Outcomes Research, Daylight saving time and early school start times cost billions in lost productivity and health care expenses. March 11, 2025.
Cleveland Clinic, Sleep Apnea: What It Is, Causes, Symptoms & Treatment. January 15, 2025.
American Medical Association, What doctors wish patients knew about sleep apnea. April 1, 2022.
Johns Hopkins Medicine, Obstructive Sleep Apnea. Accessed August 28, 2025.
Healthy Trucking of America, Sleep Apnea in Trucking: A Hidden Growing Risk on the Road. Accessed August 25, 2025.
University of Buffalo, More Black men have been dying from sleep apnea than white people and Black women. May 4, 2022.
Journal of Clinical Sleep Medicine, Ethnic/racial and sex disparities in obstructive sleep apnea among adolescents in southern California. October 1, 2024.
Rotenberg et al. Trends in CPAP adherence over twenty years of data collection: a flattened curve. Journal of Otolaryngology Head and Neck Surgery 2016; 45:43
Weaver, TE, Sawyer, AM. "Adherence to Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea: Implications for Future Inventions." Indian Journal of Medical Research, 2010; 131: 245-258.
ADHERE Registry: Data on File.
Data on file.
ACOEM, High Risk of Obstructive Sleep Apnea in Commercial Drivers. June 19, 2017.
Federal Aviation Administration, Guide for Aviation Medical Examiners. October 25, 2023.
Healthy Trucking of America, How To Avoid Truck Driving Accidents Caused By Sleep Apnea? Accessed August 25, 2025.
Mount Sinai, Frequently Asked Questions, Accessed August 27, 2025.
National Safety Council, Cost of Employee Sleep Disorders. Accessed August 25, 2025.
Overdrive, No new sleep apnea guidance in FMCSA handbook for DOT docs. January 19, 2024.
PMC, The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature. March 31, 2025.
ScienceDirect, Association between obstructive sleep apnea and multiple involuntary job loss history among recently unemployed adults. February 2021.